By Frangiska Mylona,
In the medical news, there is a common headline stating that a new ground-breaking oncologic drug has been developed, and many readers assume that this drug will provide a cure for all cancer patients. This is a misconception regarding cancer treatment. Although research with the potential to develop new medications against neoplasms is a thriving field in oncology, these drugs will not be effective for all types of cancer. In general, treatment in oncology is described as a multidisciplinary process that is based on many types of therapies including drugs, surgical procedures, and other methods in order to be effective while following the tumor’s biology.
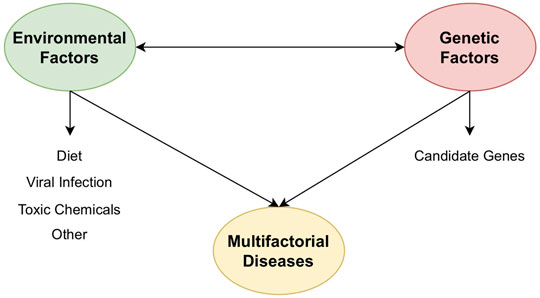
Overall, cancer is a multifactorial disease characterized by uncontrolled proliferation of cells that have escaped the body’s normal control mechanisms, which allows them to divide unmanageably. By using the term multifactorial, it means that this disease depends not only on the patient’s genetic profile but also on the environmental factors along with the patient’s habits. This is why people inherit the predisposition to develop cancer and not the cancer itself.
A simple definition for tumor formation could state that it is a mass of tissue where its cells are purposelessly, abnormally, and excessively proliferated as a result of the accumulation of genetic mutations over a period of time, which are undetected or unfixable by the body’s normal regulatory mechanisms. Some of the most common mutations involve the activation of proto-oncogenes to oncogenes or the inactivation of tumor suppressor and DNA repair genes.
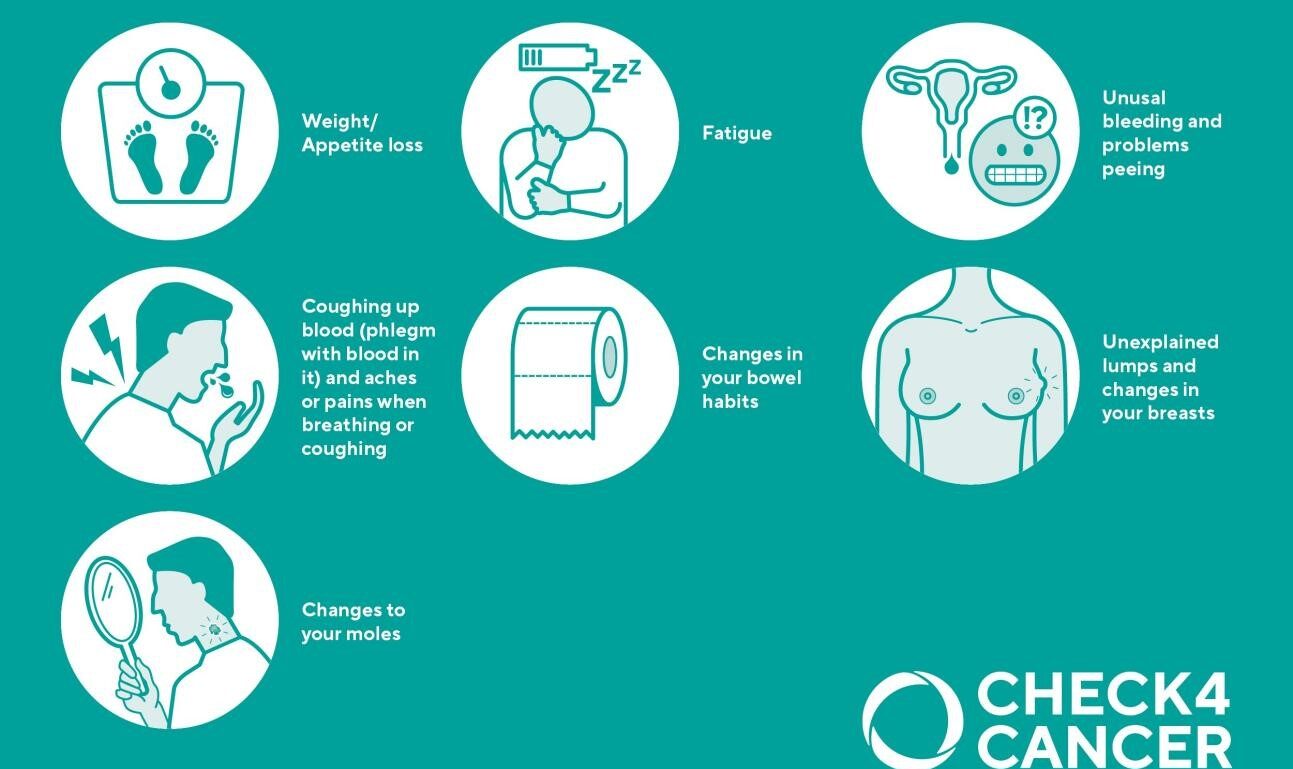
In order to diagnose and subsequently treat this complex disease, a team of many doctors with different specialties must work together, including surgeons, oncologists, radiologists, general pathologists, as well as other healthcare professionals. The first step for the correct diagnosis is a sufficient medical history and adequate physical examination. Common symptoms that could indicate the presence of a neoplastic lesion are: unexplained weight loss, fatigue, as well as other very alarming signs, including hemoptysis (which is usually an indication for lung cancer) and also abnormal swelling or abnormal lump formations, a very common indication regarding breast carcinoma.
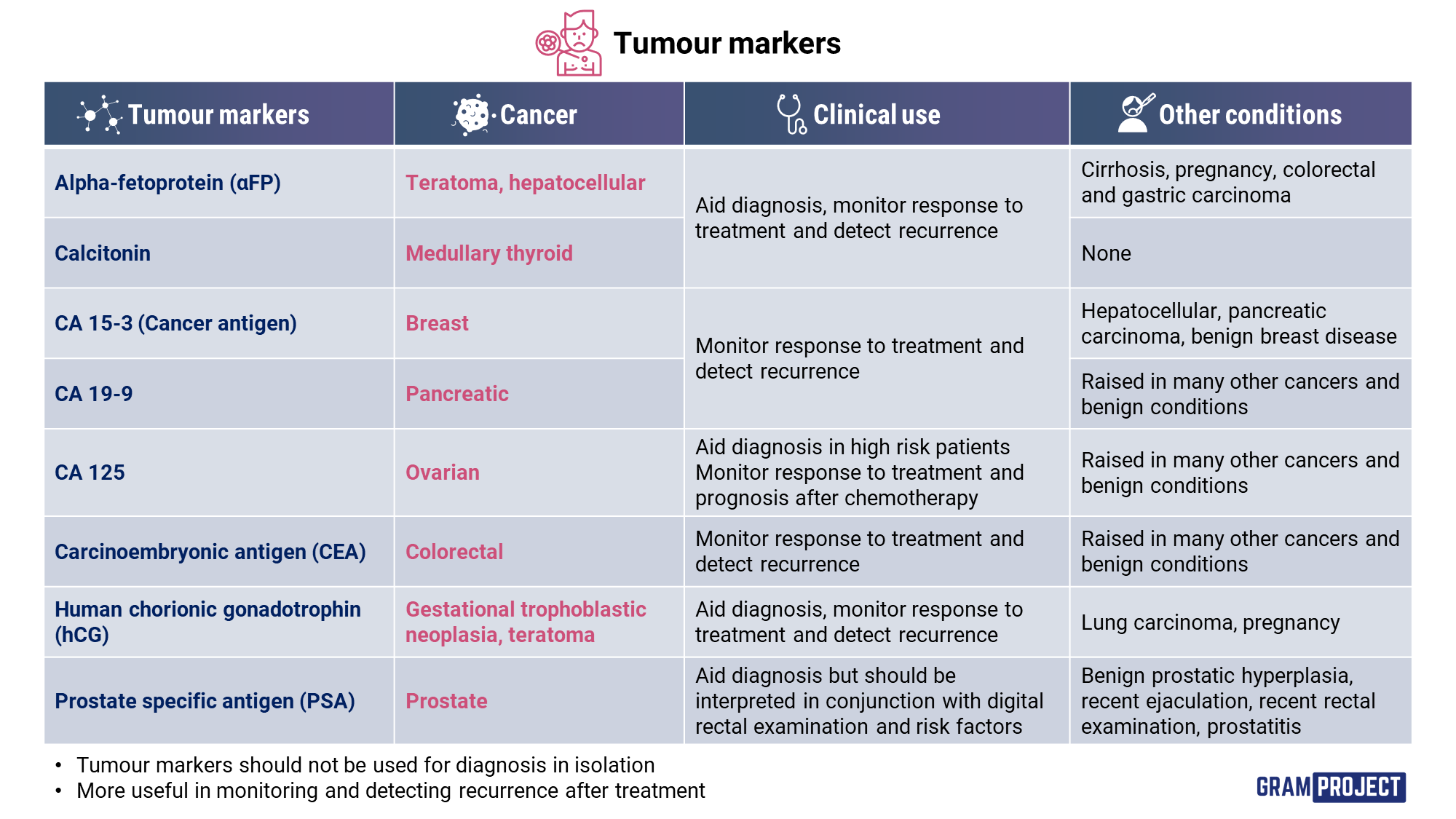
Subsequently, the next step will involve the visualization of the lesion by imaging modalities like X-rays, CT, MRI, etc. Additional laboratory tests need to be conducted, including total blood count along with other findings to determine the function of the internal organs, as well as the available tumor markers for the suspected tumor, although their elevation should not be used solely for the diagnosis since they can be elevated for other reasons apart from the presence of tumors. For instance, a common tumor marker is αFP (alpha-fetoprotein), specifically for hepatocellular carcinoma or PSA (prostate specific antigen), where its elevation may be an indication of prostate cancer.
However, one of the most important steps that will determine the type of tumor and thereafter will help in the correct treatment plan is biopsy, which will lead to establishing the tumor’s stage. Biopsy is a major step in the confirmation of the diagnosis, as well as a major component for the correct staging, and is conducted by a general pathologist. The tumor should be checked both histologically and immunohistochemically. Histology will provide an important insight that not only will classify the tumor as benign or malignant, but it will give great detail regarding its macroscopic and microscopic appearances.
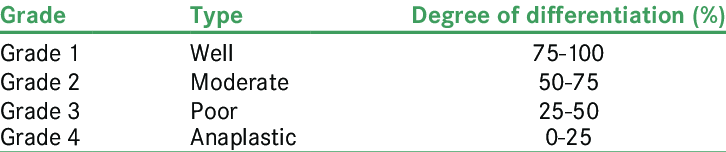
Grading is one system that expresses the tumor’s microscopic characteristics based on the degree of anaplasia and the rate of its growth. It is a beneficial system mainly for the diagnosis plus for the treatment approach. Differentiation describes the extent of resemblance of the tumor cells with the normal tissue, both morphologically and functionally. Highly differentiated tumor means that its cells resemble the normal tissue cells a lot, while poor differentiation, or even worse, anaplastic, means the opposite and it is usually more common in malignant tumors. However, its main difference with staging is that grading is based on the tumor’s pathology, while staging is based on clinical grounds.
One common way to grade tumor stems is the Broder’s system, dividing them into four categories (Grade I to Grade IV). However, there are some drawbacks concerning it. The first one is subjectivity and also the different degrees of differentiation that separate areas of the same tumor may have. To overcome this obstacle, general pathologists may report the tumor with descriptive terms.
The second thing considering biopsy is immunohistochemistry. It is a vital step and works in a pretty straightforward way, by using antibodies to stain tissue samples, where the antibodies will get attached to tumor cells, since cancer cells are regarded as antigens. One of the main data that the general pathologist will conclude out of this examination is the tumor’s origin by understanding if it is a primary tumor or a metastatic one.

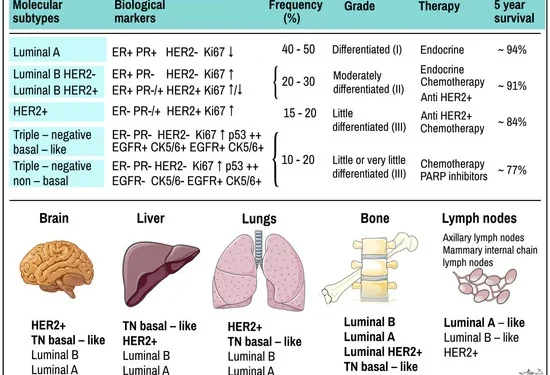
Another chief examination regarding tumors is molecular testing. Molecular testing has a major role in treatment planning, where these markers are routinely examined, with the aid of immunohistochemistry, for a better understanding of the tumor’s biological profile. Its results will “unlock” the possibility for the doctor to administer specific types of treatment, like targeted therapy. For example, targeted therapy can be given to breast carcinomas that are positive for the HER-2 marker, of Ki67 or HR (ER and/ or PR) positive. However, this treatment will not have an effect over the triple negative (TN) breast carcinomas, that tests negative for the aforementioned types of molecular markers.
Hence, it is understood that staging is based on three important criteria; the clinical examination, on other investigations including the results from the imaging modalities, as well as of the laboratory findings, and last but not least, biopsy. Nowadays, staging is confirmed by modern imaging techniques like CT, MRI or nuclear medicine tests like PET. There are two main staging systems; the TNM staging and the AJC staging.
The TNM acronym stands for: T for the primary tumor characteristics, N for the regional lymph nodes involvement and lastly, M for distant metastasis. Generally, T extends from T0 to T4 (with T4 demarcating the most malignant tumors while Tis showing carcinomas in situ), N extends from N0 to N3 (where N3 expresses extensive regional lymph node involvement) and M extends from M0 to M2 (where M2 describes large-scale distant metastasis).
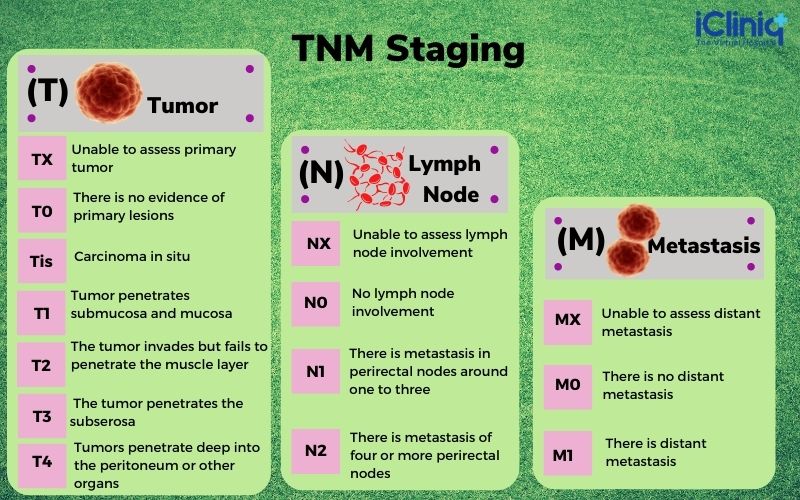
At the same time, the American Joint Committee categorizes all tumors into five stages (Stage 0 to Stage IV) which can also be divided into subcategories like Stage IIb etc… This system takes also into consideration the main components of the TNM system. For example, Stage 0 are considered early tumors with a T1, N0, M0 state.
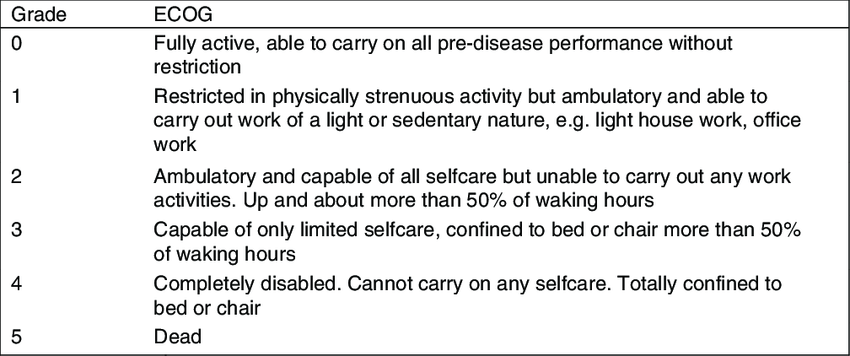
It is clear that in order to decide for the appropriate treatment, some vital steps need to be conducted beforehand. After staging, the physician needs also to take into consideration some additional parameters regarding treatment like the ECOG criteria.
The ECOG criteria are based on the ECOG scale and they represent the patient’s performance status, meaning that they delineate the ability of the patient to take care of themselves, including their daily and physical activity. The grades extend from Grade 0, where the patient is fully capable to look after themselves, to Grade 5, where the patient is dead. An important component regarding the ECOG scale are the laboratory findings, since the physician needs to know how possible is for the body to withstand the treatment.
It is necessary for the doctor to accompany all of these approaches with respect to the wishes of the patient, because oncologic treatment is a complicated process with serious side effects. A synergistic relationship should exist between the physician and the patient, with the former respecting the boundaries and desires of the patient and the latter respecting the knowledge and effort of the physician. In order to ensure that the treatment will be successful and that the patient thrives, it is imperative to recognize that cancer is a disease with distinct and unique characteristics and biology for every patient, and it requires the appropriate delicacy and the apt steps to be followed.
References
- Harsh Mohan, Ivan Damjanov. Textbook of Pathology + Pathology Quick Review and MCQs. Jaypee Brothers Medical Pub. New Delhi. 2014.
- Introduction to Medical Oncology. Epidemiology, Oncogenesis, Multidisciplinary approach in the treatment of solid tumors. Lectures from the Oncology department of the Medical University of Sofia.
- Immunohistochemistry. Cleveland Clinic. Available here




