By Frangiska Mylona,
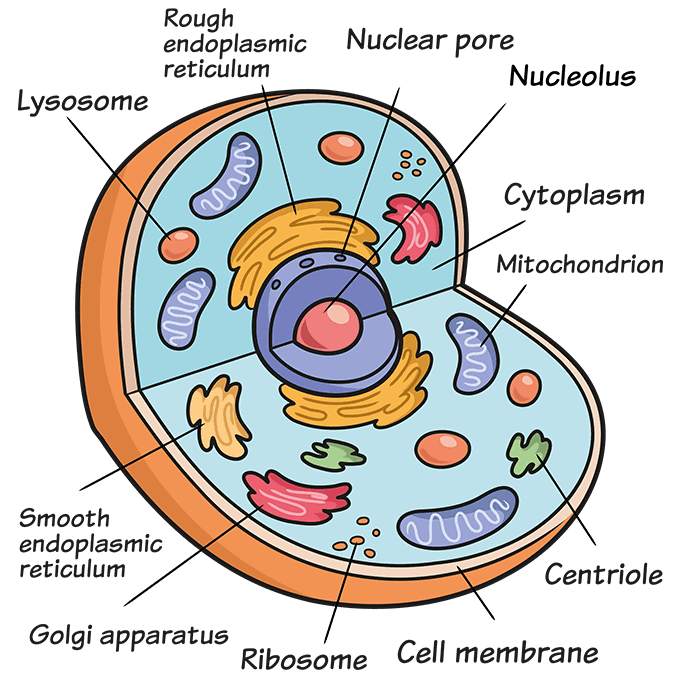
In most organisms, the cell is the smallest functional unit with the basic characteristics of life. The human body contains eukaryotic cells which combine in order to form tissues which in turn form organs. It is estimated that the number of cells in the human body reaches a trillion. Cells have some common characteristics even though they have different structures and functions depending on their location. In simple terms, the cell consists of a membrane that surrounds the cell’s cytoplasm in which the cellular organelles are ‘’bathed’’. The nucleus is surrounded by its own double-layered, nuclear membrane that separates it from the cytoplasm. The nucleus is the structure that includes the cell’s genetic information.
Cells play a fundamental role in maintaining the organism’s homeostasis. Simply, homeostasis refers to the ability of the cell, and subsequently of the organism, to keep its internal environment stable despite external changes. For example, cellular membranes have the ability to regulate homeostasis by controlling which substances enter or exit the cells.
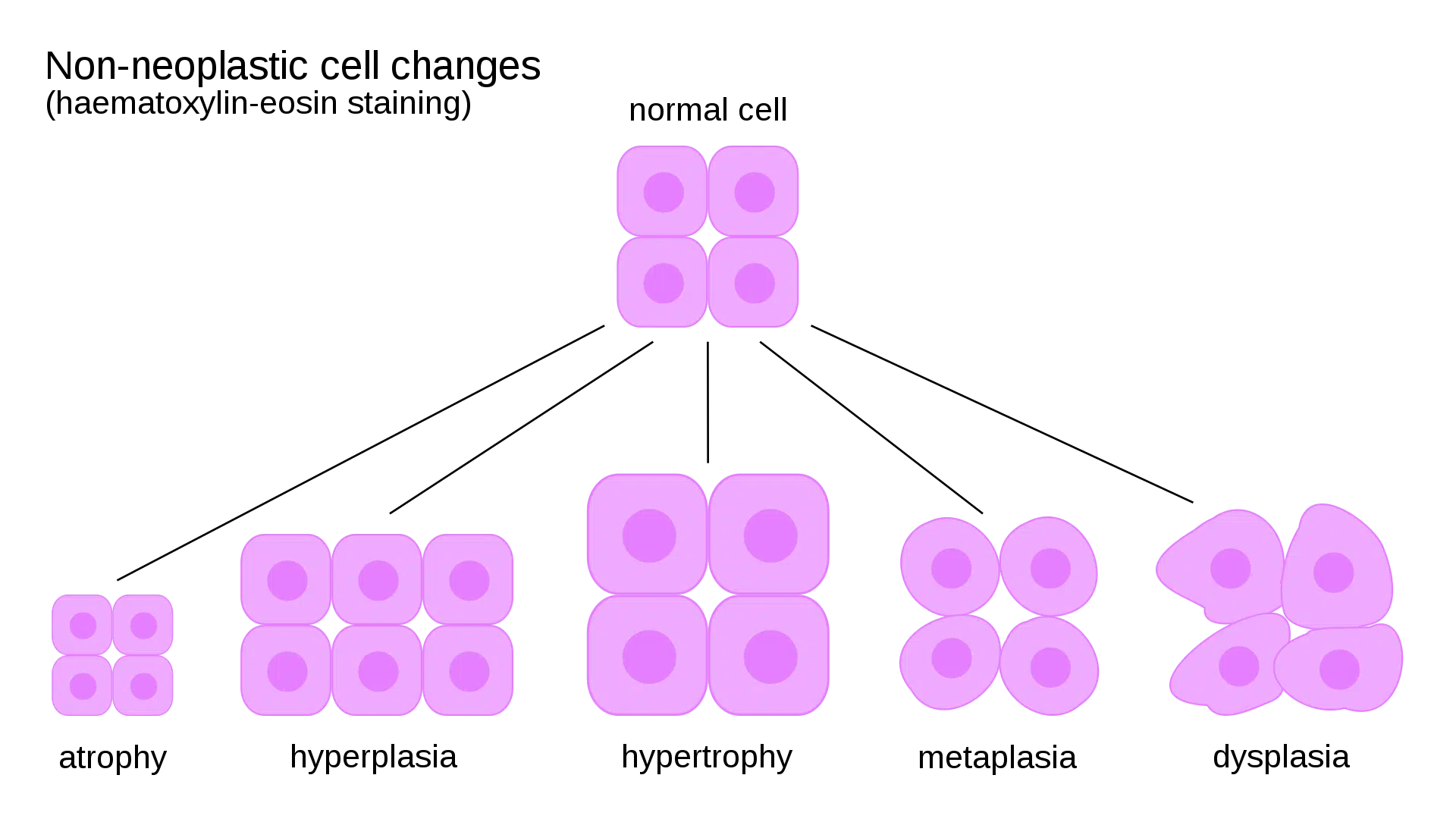
A fascinating aspect of cell behavior is its ability to adapt to adverse environmental conditions. The adaptation process can be physiologic or pathological. In general, cellular adaptation can be a potential reversible change in response to the environmental changes. The morphological adaptations observed at the cell level are the following:
A) Atrophy; is the state where cell’s (and organ’s) size decreases. There are many etiologic factors leading to this situation ranging from immobilization, malnutrition, aging, ischemia, or even due to lack of hormonal or neural stimulation. When these cells are observed under a light microscope, they are viewed as small shrunken cells.
B) Hypertrophy; is the increase in cell size and its functional ability. It can be a result of physiological processes like the hypertrophy of muscle cells during weight lifting, due to endocrine stimulation of organs during puberty or it could be a pathological change f.e. the hypertrophic cardiac muscles during hypertension.
C) Hyperplasia; refers to the increase in the number of cells in a tissue or an organ. However, some cells cannot exhibit this feature like nerve cells. Again, it can be physiologic for example due to hormonal stimulation (such as the development of breast tissue during puberty), or pathologic like the hyperplasia of the prostate gland due to aging.
D) Lastly, metaplasia; refers to the reversible change of one cell type to another as a response to irritation. Apparently, this change makes the cell more resilient to environmental stress. An interesting example is seen in the bronchial epithelium of tobacco smokers.
If the cell is unable to adapt, it will lead to cellular injury. Cellular injury is divided into two types; reversible cellular injury and irreversible cellular injury. The reversible injury can, eventually, pass and the cell will return to its normal state, however, the irreversible cell injury leads to cell death via either apoptosis or necrosis.
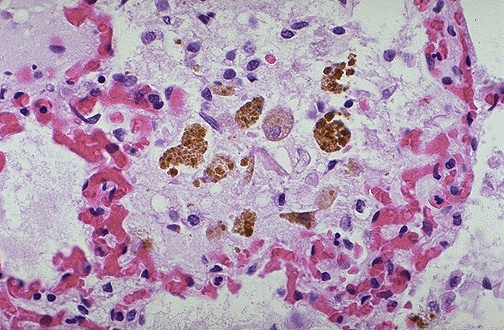
Apart from the aforementioned cellular changes, during cellular injury pathological accumulations of substances can be observed. Some of the pigments are lipids and proteins, such as those found in the proximal tubules in the kidneys leading to proteinuria.
Other pigments include hemosiderin, a yellow-brown pigment seen during hemorrhages and bruises. Additionally other include, melanin, bilirubin, and lipofuscin, a wear-tare pigment seen most commonly in the liver and heart.
Furthermore, lifestyle and pollution can cause exogenous substances to accumulate. For instance, in the lungs are frequently observed anthracotic pigments, and even tattoos are considered exogenous pigments.
There is a plethora of causes that can lead to cell injury. The most common is hypoxia, which occurs when cells lack oxygen and cannot synthesize critical molecules like ATP. ATP (or the adenosine triphosphate molecule) is responsible for providing the tissues with energy. One of the causes of hypoxia is ischemia, where the tissues are deprived of blood supply due to atherosclerosis, thrombus, or thromboembolism.
Other causes include injuries from pathogens like viruses and bacteria, hypersensitivity reactions like allergies as well as injuries from chemical factors like drugs (cyanide), pollution, or even occupational exposure (like carbon monoxide and asbestos). Physical injuries can also cause cellular damage including burns, wounds, frostbite, and of course, radiation.
Health and lifestyle play a crucial role in the development of cellular injury. Alcohol consumption, smoking, and drug abuse are some of the most familiar examples. Also, decreased protein and calorie intake may lead to marasmus while the opposite scenario like excessive calorie intake may lead to obesity, atherosclerosis, and even sudden death.
Particular interest arises regarding vitamins that protect the cells from injuries. Nowadays, fast food and nutritional deterioration have resulted in their neglect and disregard. For instance, Vitamin D deficiency can lead to fragile bones, rickets and osteomalacia. Vitamin K deficiency can lead to easier bleeding, vitamin A deficiency is associated with night blindness as well as if a pregnant woman is deficient in folate (Vitamin 9), it can result in neural tube defects in the embryo like spina bifida. However, it is worthwhile to remember that excessive vitamin intake (hypervitaminosis) can result in tissue-specific abnormalities, but it is a rare problem in our days.
All these factors that lead to cell injury usually interfere with the DNA, with the cellular permeability (due to cell membrane damage) leading to the deprivation of the organism of ATP, where its deprivation can lead to increased anaerobic glycolysis and the formation of lactic acid that will decrease the cell’s and organism’s pH. Body pH must be strongly regulated in order to maintain health. The mitochondria can also release apoptosis triggers and affect ATP production following cellular injury.
The loss of cellular membrane integrity has a significant impact on the clinical and laboratory approach to cell disease and damage. When the cellular membrane is damaged, intracellular enzymes can leak out of the cell into the bloodstream, so they will be measurable when laboratory tests are performed. Important examples include: Troponin and CPK-MB for myocardial injury, transaminases during hepatitis, amylase, and lipase during pancreatitis as well as alkaline phosphatase in case of biliary tract obstruction.
As it was mentioned before, if a cell cannot adapt, it will be subjected to injury that can lead to cell death. There are two types of cell death: necrosis and apoptosis.
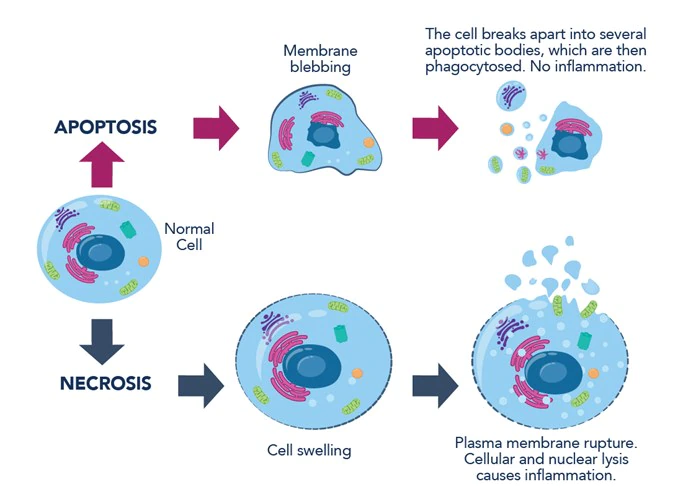
Necrosis is a passive, accidental, and unprogrammed death caused by the inability of the cells to recover from a cellular injury. It is followed by an inflammatory response.
There are many types of necrosis that are the result of different processes. When there is an ischemic injury the necrosis is coagulative. When cells are destroyed by hydrolytic enzymes, like in brain abscesses, the necrosis is liquefactive. One of the most peculiar necrosis types is caseous or ‘’cheese-like’’ necrosis. It is a characteristic type of necrosis associated with tuberculosis. Lastly, gangrenous necrosis leads to dead tissue involving most commonly the lower limbs, the testes, and parts of the gastrointestinal tract.
On the other hand, apoptosis is completely different from necrosis. It involves the programmed death of cells without causing inflammation. It is an active process due to cell injury and DNA damage that is regulated by proteins like protein p53. This protein detects DNA damage that cannot be repaired and stimulates apoptosis. If this specific protein is defective, it can lead to cancer. Physiological examples of apoptosis include the menstrual cycle or can be seen during embryogenesis. Particularly, if the cells in the interdigital space fail to undergo apoptosis the fetus will be born with webbed hands or feet, a disorder known as syndactyly.
In general, it is easy for a cell to get injured either by aging, which is an inevitable process that degrades the cell condition, or by poor lifestyle choices. Despite that, it is essential to understand the mechanism that can kill a cell and to realize that by adopting a healthier lifestyle, cell injury risk can be reduced.
References
- USMLE® , Step 1 , Pathology lecture notes 2018. Kaplan medical.