By Frangiska Mylona,
The announcement of pregnancy and the birth of a baby are happy events. This is celebrated by both the parents and the whole family of the newborn. During these nine months of pregnancy, the mother will visit a number of doctors and specialists. These doctors will reassure her that her fetus or even fetuses will be born healthy and strong. However, it is not unusual to hear that there is the possibility of a preterm birth meaning before the 37th week of pregnancy has been completed. In contrast, normally the birth of a baby is expected around the 39th to the 40th week of pregnancy. This announcement can be frightening for many reasons but one of the most terrifying and significant ones involves the immature lung development of fetuses.
It is obvious enough that the lungs are very special organs that are mainly involved in the process of respiration that facilitates the gas exchange where the oxygen is inspired and transported throughout the body while the carbon dioxide is eliminated out of the body into the environment with each expiration and the ventilation process that involves the mechanical movement of air into and out of the lungs.
Apart from the lungs, there are also other organs that aid in these processes. These organs are separated into two categories:
1) The organs of the upper respiratory tract including the:
- Nose and the respiratory part of the nasal cavity
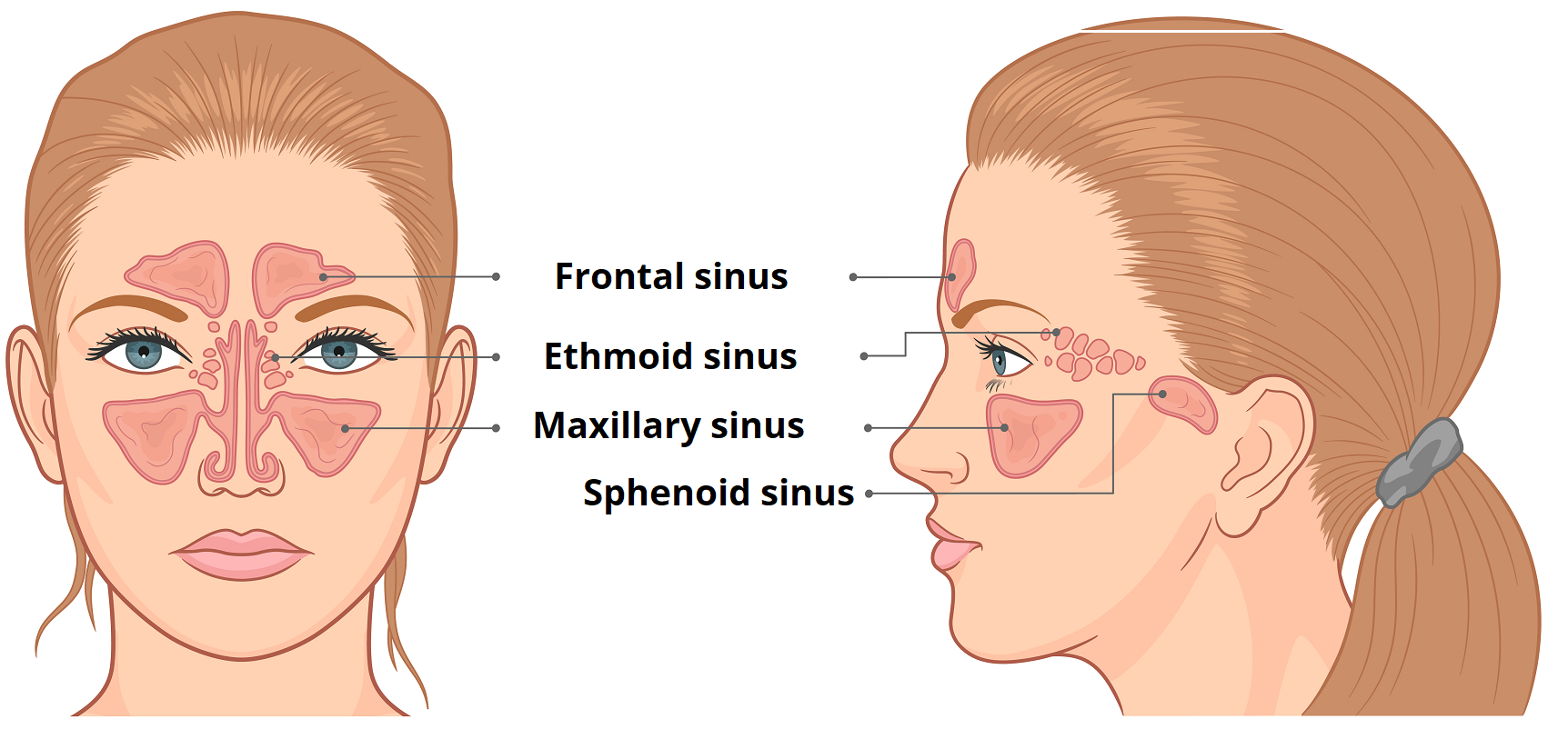
- Paranasal sinuses. These are hollow spaces around the nose located in the frontal, ethmoid, sphenoid, and maxillary bones. Their function is to decrease the relative mass of the skull. They also humidify and warm the inhaled air and they also are involved in the sound resonance process. They are connected to the conchae of the nasal cavity by the meatuses.
- Pharynx, which is divided into the nasopharynx, oropharynx, and laryngopharynx
- The upper part of the larynx, including the epiglottis, keeps the larynx open during respiration so that air can pass through.
2) The organs of the lower respiratory tract including the:
- The inferior portion of the larynx
- Trachea is the continuation of the larynx. It gives rise to the right and left primary bronchi which enter the lungs (through the hilum or root of the lungs) that subsequently give rise to the lobar and segmental bronchi. These bronchi subsequently divide into the terminal bronchioles which give off the respiratory bronchioles that end as alveolar sacs and ducts filled with alveoli. These alveoli are the sites of gas exchange and are surrounded by pulmonary capillaries. The oxygen from the alveoli is diffused into the capillaries and the carbon dioxide is released from the capillaries to the alveoli in order to be breathed out.
- Lungs where the right lung is divided into three lobes while the left lung is divided into two lobes due to the presence of the heart. Each lung is surrounded by the pleura which is further subdivided into the visceral and the parietal pleura with the pleural cavity in between containing a serous fluid (approximately 15 ml) that permits the smooth movements of the lungs and pleura during breathing and ensures the negative pressure in the thoracic cavity to keep the lungs under tension and able to perform the ventilation process.
In the process of ventilation, it involves two groups of muscles:
1) The muscles of inspiration in which the diaphragm is principally involved, as well as the external intercostal and the accessory muscles which can be utilized during exercise or in respiratory distress syndromes.
2) The muscles of expiration involve the abdominal muscles and the internal intercostal muscles.
Additionally, functionally the respiratory system is divided into the conducting zone including the organs that are not directly involved in the gas exchange process such as the nose and the nasal cavity, the pharynx, the larynx and the trachea, and the respiratory zone that it is involved directly in the gas exchange including the respiratory bronchioles, the alveolar sacs, and ducts containing many alveoli.
In order for pulmonary ventilation to be successful, it is dependent on three types of pressures;
- The atmospheric pressure
- The intra-alveolar pressure (intrapulmonary pressure)
- The intrapleural pressure.
The three of them are based on the concept of negative and positive pressures where the reference point is always the atmospheric pressure. Generally speaking, any pressure below the atmospheric one is referred to as negative, while any pressure above it is referred to as positive. Thus, in order for the lungs to function properly, the intrapleural pressure needs to remain lower (or negative) than the intra-alveolar pressure. The latter is equal to the atmospheric pressure at rest. In contrast, it becomes slightly negative during inspiration where air flows into the lungs and transforms into slightly higher than the atmospheric pressure during expiration.
For the sake of this process, it is normal for the lungs to follow two very crucial concepts. This will help them not to collapse during this change of pressure and to actively participate in the gas exchange process. The first concept describes compliance. This is generally referred to as the ability of an organ to be stretched based on its elasticity and the surface tension that can act as an inward force. This force tries to reduce the alveolar surface area exposed to the air and therefore tries to make the alveoli collapse. This is the point where a premature birth could be fatal because the alveoli are made of cells that even during the fetal period, produce a vital substance named surfactant. This substance reduces the surface tension in the alveoli so that they do not collapse during respiration.
Specifically, for the embryogenesis of the lungs, they are derived from a part of the embryo known as the primitive gut tube or foregut which will also give rise to many gastrointestinal organs. Around the 4th gestational week, an out-pocketing appears in the proximal part of the primitive gut tube known as the respiratory diverticulum. Initially, the respiratory diverticulum is continuous with the posterior gut tube that will develop as the esophagus. However, in order for both the respiratory and gastrointestinal organs to be functional, it forms a ridge termed the tracheoesophageal septum that separates the developing lung bud from the esophagus. The lung bud gives rise to the bronchial bud which will continue to grow and mature until the eighth year of age.
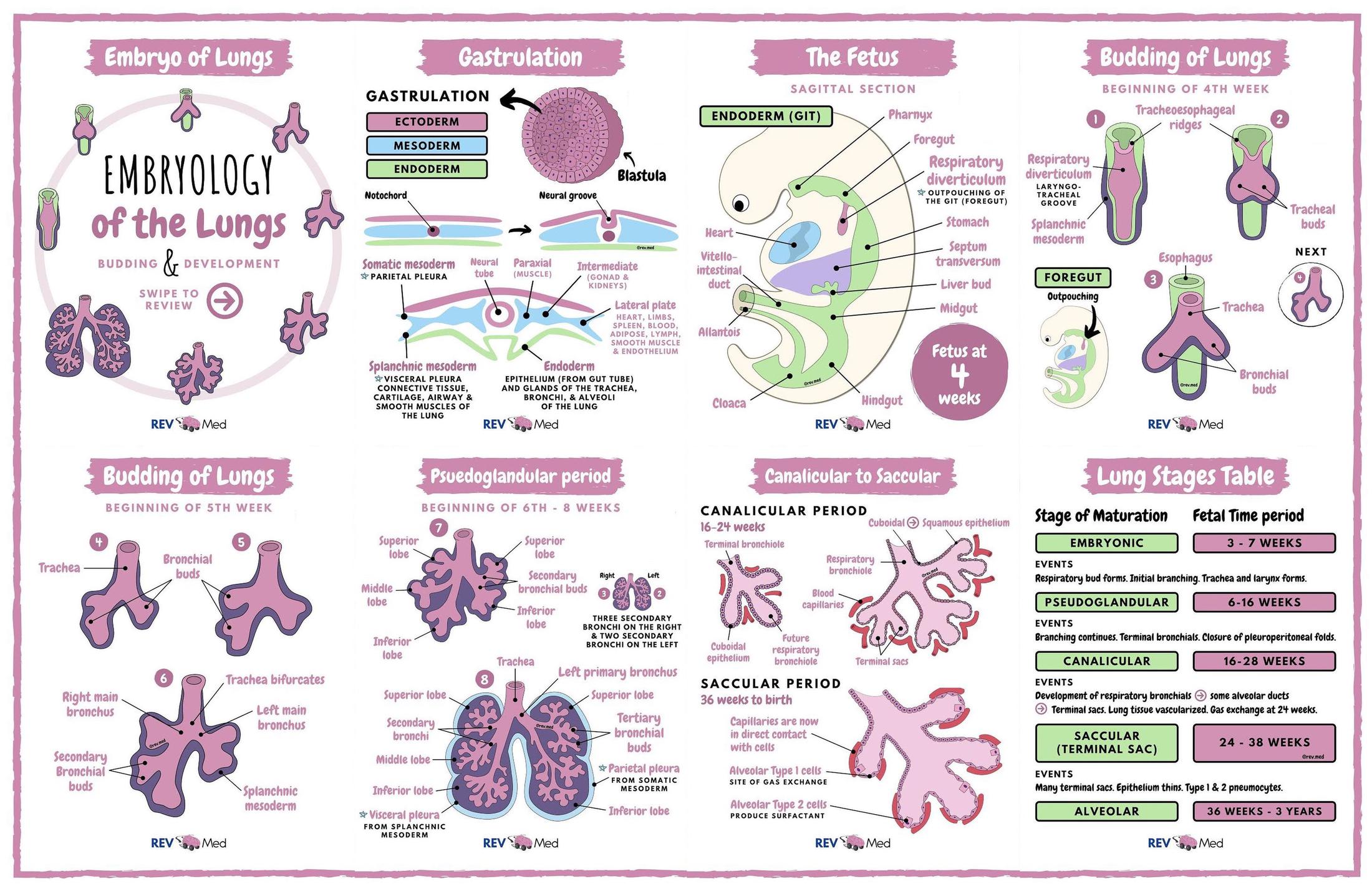
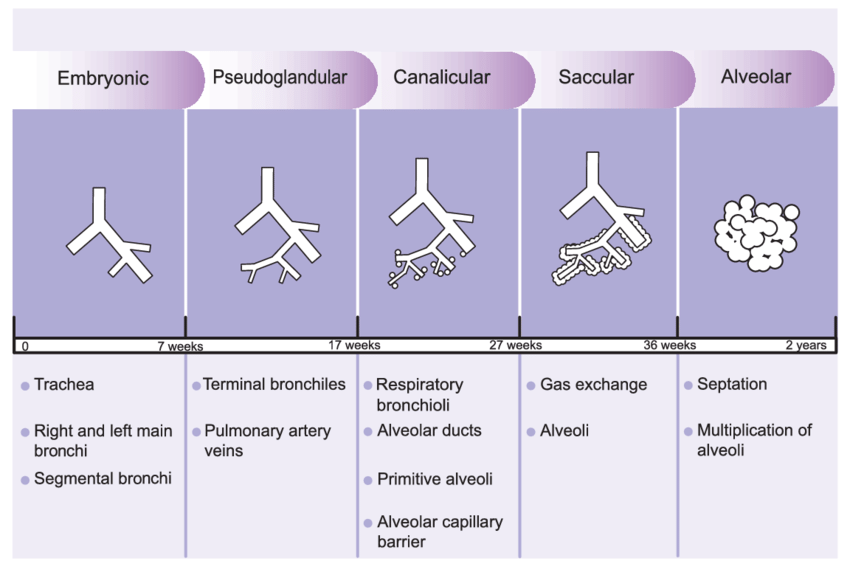
This development is divided into four stages where:
1) From the fifth week of gestation till the 16th week, it is known as the first or the pseudo glandular stage, where the bronchial bud gives rise to the right and left primary bronchi that will divide into the lobar bronchi, then to the segmental or tertiary bronchi and lastly, to terminal bronchioles.
2) From the 16th gestational week till the 26th gestational week, this second stage is known as the canalicular stage where from the terminal bronchioles, the respiratory bronchioles are developed breaking off to the smaller respiratory units which are the alveolar sacs and ducts that include multiple alveoli. From a histological point of view, the alveoli are primitive at that stage made from cuboidal cells that due to their size, the alveoli are still not ideal for the gas exchange process.
3) From the 26th week of gestation until birth, this stage is known as the saccular stage characterized by an increased amount of respiratory bronchioles and alveoli. At this point, type 1 pneumonocytes will be formed. They can facilitate the gas exchange process because, from a histological point of view, they are composed of thin, simple squamous cells allowing the gas exchange process more than the previous cuboidal cells. Also, type 2 pneumonocytes are composed of cuboidal cells responsible for producing and releasing surfactant. The surfactant is composed around the 24th to 35th week of gestation but after the 35th week, it is produced in significant amounts. The surfactant is composed of a specific phospholipid known as the DPPC (dipalmitoylphosphatidylcholine) that accounts for its surface tension-reducing properties that help the alveoli not to collapse during respiration, and of the surfactant proteins such as SP–A, SP–B, SP–C and SP–D that help organize the surfactant layer and modulate the alveolar immune responses. Additionally, hormones such as cortisol, insulin, prolactin, and thyroxine modulate surfactant production.
During the preparation for the birth, the fetus breathes amniotic fluid to prepare its lungs for the first birth.
At the time of birth, the amniotic fluid is absorbed by the pulmonary capillaries that surround the alveoli and the type 2 pneumonocytes produce surfactant. When the baby is born it must cry immediately because that first cry indicates that the alveolar sacs, alveolar ducts, and therefore the alveoli have opened successfully. Therefore the lungs are ready to function properly.
4) From the 36th week of gestation till the 8th year of age, it is known as the 4th stage or as the alveolar stage where the alveoli mature and are separated from each other by septa. Around the time of birth, there are almost 100 million alveoli while around the age of eight around 300 million alveoli are estimated.
Regarding neonatal distress syndrome, if the fetus is born prematurely around the 26th to 27th week of gestation the type 2 pneumonocytes are not matured enough to produce enough surfactant therefore the alveoli will collapse and will not be able to open, leading to the inability to breathe and to the manifestation of this syndrome.
There are also cases of newborns that are at higher risk, including:
- Twin or multiple births since, sometimes, they are born prematurely
- C–section (cesarean) delivery of babies before the baby is full-term
- The mother has diabetes
- Problems with the delivery that reduces blood flow to the baby
- Even hypothermia due to the fact that the baby cannot keep its body temperature warm at birth.
Infants with neonatal respiratory distress syndrome exhibit the following clinical features:
- Fast breathing very soon after birth
- Changes in the color of lips, fingers, and toes
- Widening of the nostrils with each breath
- Chest retractions.
The diagnosis is based on the bay’s clinical image along with the results of chest X-rays and blood tests.
The treatment needs to be urgent by supplying the baby with extra oxygen either by a nasal cannula which is a small tube that is placed into the nostrils providing oxygen or even by placing the baby on a Continuous Positive Airway Pressure (CPAP); this machine gently pushes air or oxygen into the lungs to keep the air sacs open. In severe cases, a ventilator is used to help the infant breathe when they are incapable of breathing independently.
In extremely premature infants, the prophylactic administration of exogenous surfactant can be given in order to reduce the risk for neonatal respiratory distress syndrome. Moreover, when a mother is suspected of premature delivery, cortisol can be administered, thereby reducing the risk of neonatal mortality.
In conclusion, the breathing process may seem simple and natural, however, the human body engages such complex mechanisms in order to accomplish these vital functions. As such, it is essential to realize how valuable every breath is and subsequently that one of the greatest achievements in a human’s life is their first breath, which grants them a long, healthy life and strong, functional lungs.
References
- Moore’s Essential Clinical Anatomy, 6th edition, by Anne M.R.Agur and Arthur F.Dalley.
- Memorix anatomy, 1st edition, by Radovan Hudak, David Kachlik, Ondrej Volny, et al.
- Anatomy and Physiology by OpenStax (Official Print Version, hardcover, full color), first edition by Kelly A. Young (Author), James A. Wise (Author), Peter DeSaix (Author), Dean H. Kruse (Author), Brandon Poe (Author), Eddie Johnson (Author), Jody E. Johnson (Author), Oksana Korol (Author), J. Gordon Betts (Author), Mark Womble (Author).